Diagnosis and Monitoring of Age-Related Macular Degeneration (AMD) and Geographic Atrophy (GA)
Ophthalmologists and optometrists use a variety of tests and examinations to determine whether a patient may have age-related macular degeneration (AMD). This includes techniques to see the retina and the macula at the back of the eye, as well as methods to test visual function.1,2 Here, we explain the different diagnostic and monitoring tests related to AMD and one of its advanced forms, geographic atrophy (GA).
The only way to diagnose AMD or GA is to have a thorough eye examination, including a check of the macula, by an ophthalmologist or optometrist.
Overview of diagnosis and monitoring
Many of the tests used to diagnose AMD are also used to monitor a patient over time following diagnosis. Your ophthalmologist or optometrist will tell you how often you should attend follow-up visits, and it is important to follow their advice.
Some of the tests will be carried out by your healthcare professional, while you can use others to monitor your own vision.
Watch the video below for an overview of the tests used to diagnose and monitor AMD.
Monitoring your own vision: Amsler grid
If you have been diagnosed with AMD or geographic atrophy, or are at risk of developing an eye disease, it is important to ensure you are monitoring any changes to your vision.
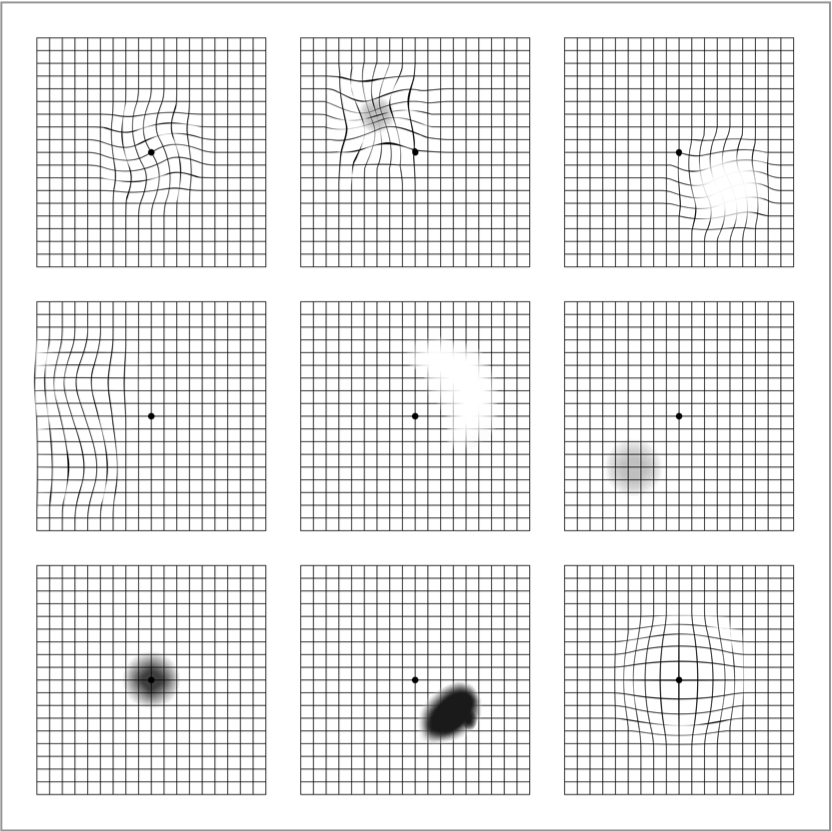
An Amsler grid is an essential and easy-to-use self-monitoring tool used to detect early vision changes. This may include distortion (straight lines appearing wavy), blurred patches or dark patches.3
It is important not to rely on an Amsler grid for diagnosis; it is not a substitute for regular eye examinations. The only way to diagnose AMD or GA is to have an eye exam, including a check of the macula, by an ophthalmologist or optometrist
Note that vision changes on an Amsler grid may indicate an eye disease other than AMD or GA.
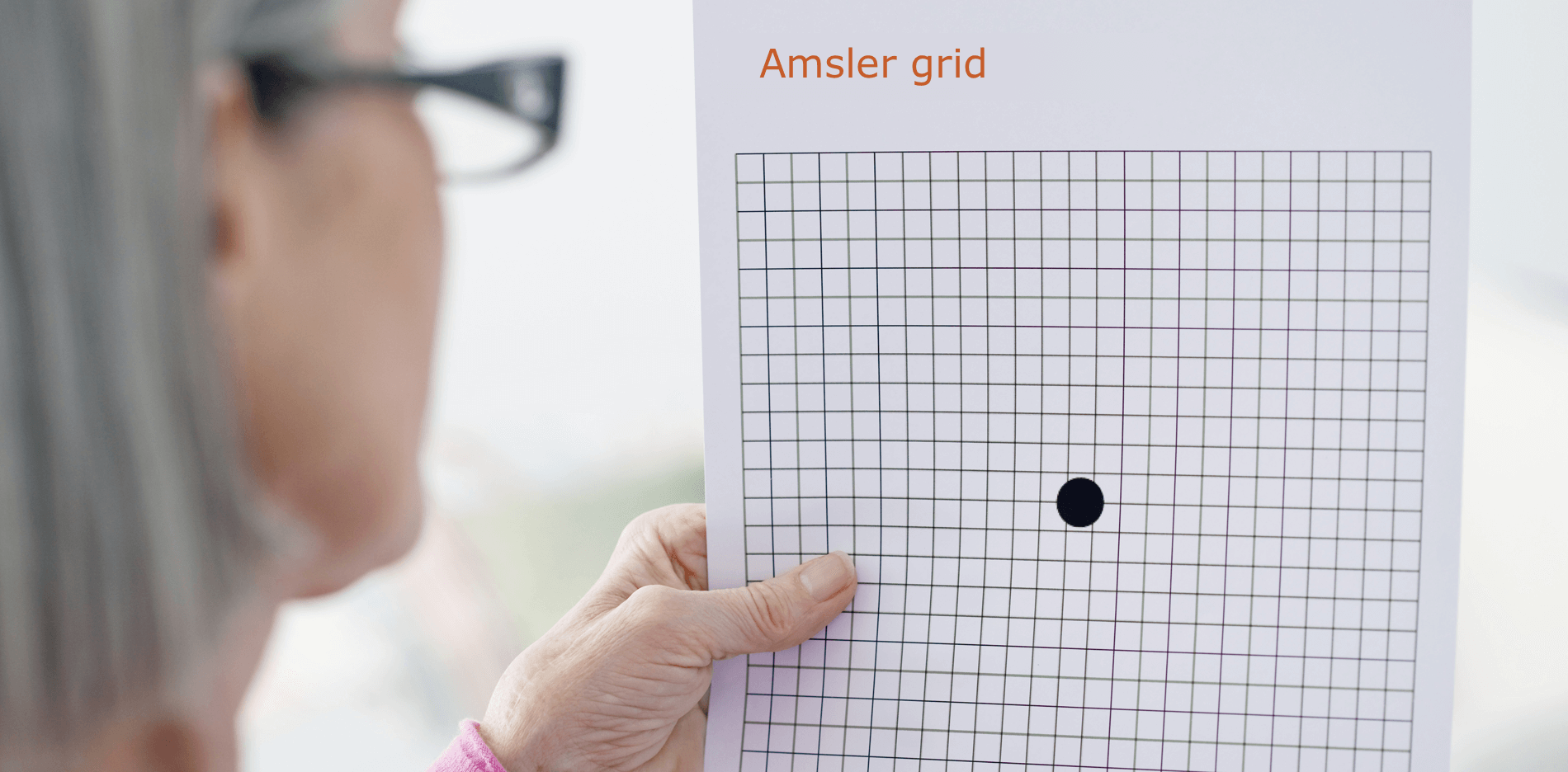
If you detect any changes in your vision, it is important to talk to an ophthalmologist or optometrist as soon as possible.
You can download and print an Amsler grid by following the link below or by visiting the Resources section of the website. This resource includes the Amsler grid as well as step-by-step instructions on how to use it to monitor your vision.
The next section provides an overview of the examinations that your healthcare provider may carry out.
Tests used to diagnose and monitor AMD or GA
Not all tests described here will be carried out by your ophthalmologist or optometrist; the tests used may differ depending on where you live. If you have any questions related to these tests, please speak to your healthcare professional at the next visit.
In general, the more common tests used are:1,2
• Comprehensive eye examination
• Fundus examination
• Ophthalmoscopy
• Fundus photography
• Optical coherence tomography
• Fundus fluoresceine angiography
• Fundus autofluorescence
Less common tests include:
• Indocyanine green angiography
• Microperimetry
• Low-luminance visual acuity
• MNRead Acuity Chart
• Contrast sensitivity examination
• Functional Reading Independence (FRI) Index
Read on for a more detailed description of some of the tests listed above.
Comprehensive eye examination
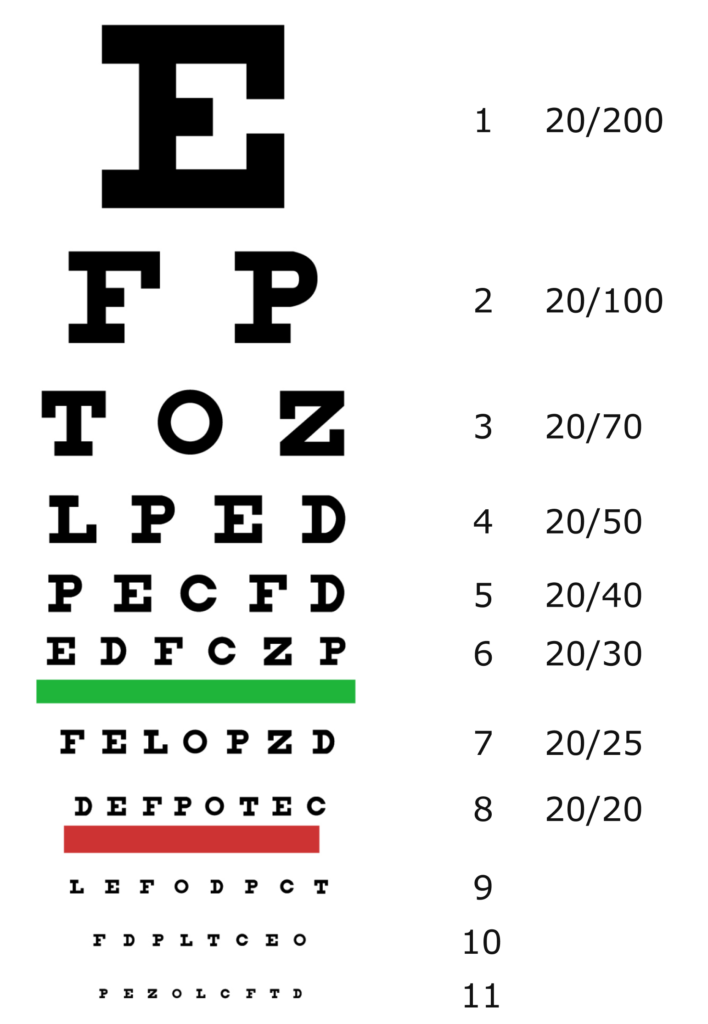
The main symptom experienced by people with AMD is vision loss. Hence, AMD is often diagnosed by a routine eye exam, which measures visual acuity – a person’s ability to see details, shapes and letters at a certain distance.4 This is normally assessed using something called a Snellen chart, though other charts may also be used. The number of letters a person can correctly identify (i.e. the further down the chart they can read) represents their visual acuity.4

Fundus examination
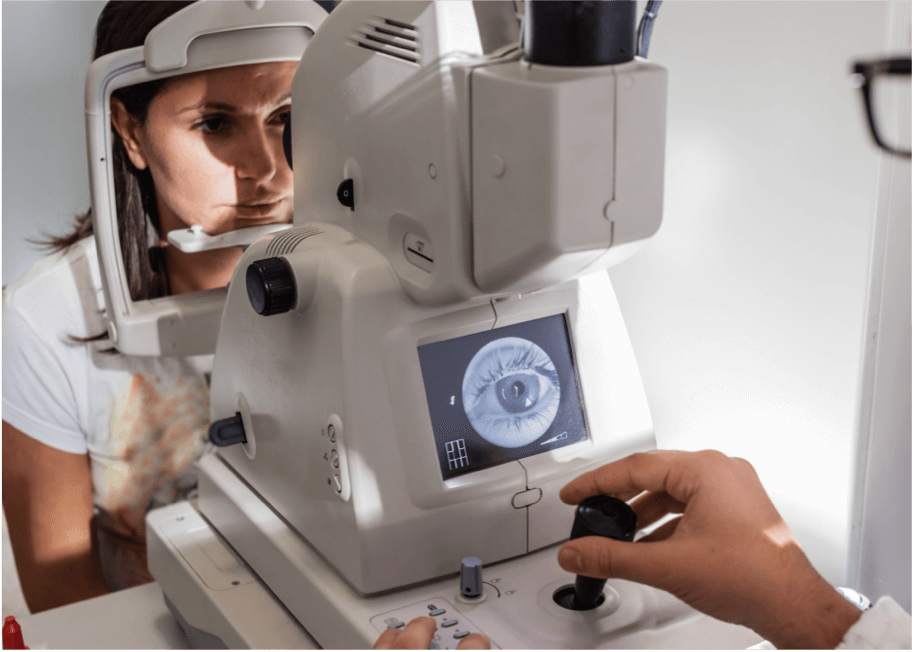
This is a more in-depth test to help diagnose AMD. It is an optical examination of the retina at the back of the eye. Note that fundus is just a medical term for the part of an organ that is furthest from the opening, and in this case, it refers to the back of the eye. The fundus examination can be conducted using either ophthalmoscopy or fundus photography. In both methods, dilating drops are applied to the patient's eye to allow the ophthalmologist or optometrist to see more of the back of the eye.1
Ophthalmoscopy
In this eye examination method, a bright light is shone through the dilated pupil and an ophthalmoscope provides magnified images of the retina. Ophthalmoscopy is an important diagnostic tool for AMD as it allows detection of any abnormalities in the eye, like atrophy (areas of damage), drusen, pigmentary (colour) changes and choroidal neovascularisation (CNV).5,6
There are three types of ophthalmoscopy:
Direct ophthalmoscopy
A bright light is shone through the pupil using a handheld ophthalmoscope.5

Indirect ophthalmoscopy
This is the most common type of ophthalmoscopy. A bright light is sent through the pupil from a head-mounted ophthalmoscope and a handheld lens is used to examine the eye.5

Slit-lamp ophthalmoscopy
This method is commonly used to diagnose AMD. The patient’s chin rests on a slit-lamp device, light is sent through a narrow slit into the patient’s eye and the fundus is examined through a magnifying glass.6

Fundus photography
This is carried out using a low-powered microscope to take colour images of the retina. It is commonly used in the diagnosis of AMD, as it shows abnormalities like drusen, pigmentary (colour) changes, atrophy, bleeding, and fluid build-up. Images taken over time can be compared to monitor the progression of the disease.2
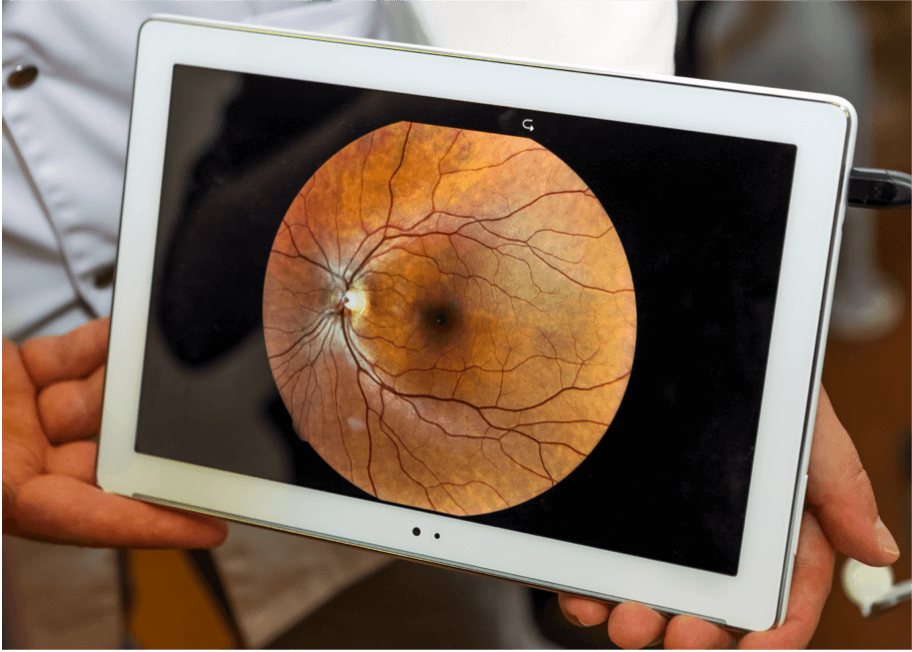
There are a number of techniques that provide a more detailed image of the retina. These techniques allow practitioners to determine the stage and severity of AMD at diagnosis, as well as monitor its progression over time.
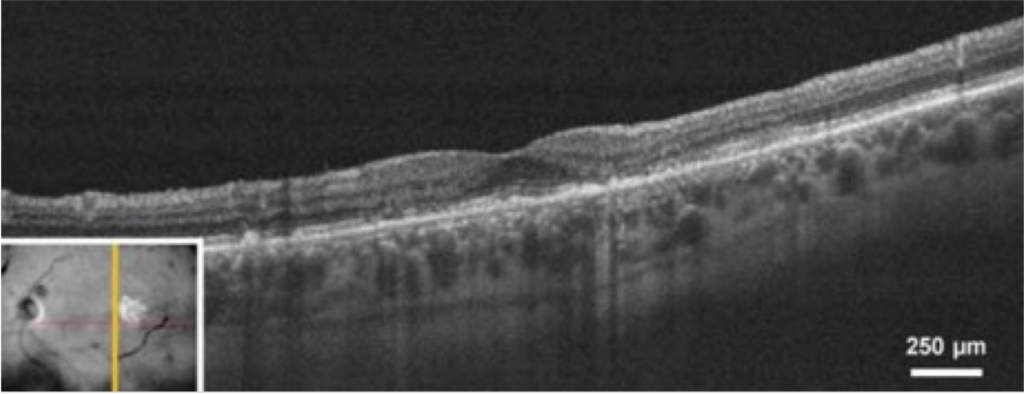
Optical coherence tomography (OCT)
OCT is an important imaging technique for diagnosing and monitoring AMD. This method involves taking cross-sectional pictures of the retina to give a detailed picture of its health.7,8

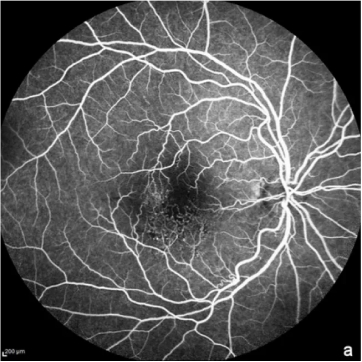
Fundus fluoresceine angiography (FFA)
Here, a fluorescent dye is injected into the vein in order to visualise blood vessels in the retina. FFA is usually used to rule out a diagnosis of wet AMD.1 It can also be used in geographic atrophy to show the regions of damage where retinal cells have died.7

Fundus autofluorescence
Fundus autofluorescence is an important imaging technique for diagnosing and monitoring AMD, particularly one of its advanced forms, geographic atrophy.1 When exposed to a specific light (normally blue), a molecule called lipofuscin in the eye produces light, or fluorescence, which can be observed. Unhealthy regions may appear darker for atrophic areas, or brighter for drusen, which are both signs of AMD.7

Access helpful resources
View the glossary section for further explanation of any unfamiliar terms used throughout this section and across the website.
References:
- BrightFocus Foundation. The eye exam for macular degeneration. 2021. Available at: https://www.brightfocus.org/macular/article/eye-exam-macular (accessed February 2024).
- BrightFocus Foundation. Retinal imaging for diagnosing and treating AMD. 2021. Available at: https://www.brightfocus.org/macular/article/retinal-imaging-diagnosing-and-treating-amd (accessed February 2024).
- American Academy of Ophthalmology. Have AMD? Save your sight with an Amsler Grid. 2020. Available at: https://www.aao.org/eye-health/tips-prevention/facts-about-amsler-grid-daily-vision-test (accessed February 2024).
- Lakshminarayanan V. Visual acuity. In: Handbook of Visual Display Technology, vol 1. Springer Berlin Heidelberg, 2012; pp.93–99.
- American Academy of Ophthalmology. What is the difference between direct and indirect ophthalmoscopy? 2018. Available at: https://www.aao.org/eye-health/ask-ophthalmologist-q/what-is-difference-between-direct-indirect-ophthal (accessed February 2024).
- American Academy of Ophthalmology. What is a slit lamp? 2018. Available at: https://www.aao.org/eye-health/treatments/what-is-slit-lamp (accessed February 2024).
- Fleckenstein M, et al. Ophthalmology. 2018;125(3):369–390.
- AMD BOOK. Optical coherence tomography in age-related macular degeneration. 2017. Available at: https://amdbook.org/content/optical-coherence-tomography-age-related-macular-degeneration (accessed February 2024).
UK-GA-2300059 March 2024